CONTEST!
Please submit your Washington University Orthopedics success story by October 15, 2013, to www.ortho.wustl.edu/mystory. We will select a story to feature on our website, and the lucky winner will receive 2 club tickets with food and beverage vouchers to the Rams vs. Titans game on November 3 -- the ultimate VIP experience!
Washington University Orthopedics in St. Louis, Missouri offers a full complement of comprehensive orthopedic services to meet your needs. For an appointment with an orthopedic specialist, call 314-514-3500.
Wednesday, September 25, 2013
Tuesday, September 17, 2013
Wine and Wisdom Event for Female Orthopedic Surgeons

 The "Wine and Wisdom" event for female orthopedic surgeons in the St. Louis community was a big success! Currently, only 4% of the American Academy of Orthopaedic Surgery (AAOS) fellows are women. The "Wine and Wisdom" event attracted 25 female orthopedic surgeons from St Louis. The purpose of the event was to provide support, mentorship and advice for each other and for trainees in the field of orthopedics.
The "Wine and Wisdom" event for female orthopedic surgeons in the St. Louis community was a big success! Currently, only 4% of the American Academy of Orthopaedic Surgery (AAOS) fellows are women. The "Wine and Wisdom" event attracted 25 female orthopedic surgeons from St Louis. The purpose of the event was to provide support, mentorship and advice for each other and for trainees in the field of orthopedics.
Monday, June 24, 2013
ACL Injury Prevention Tips
ACL INJURY RATES
The anterior cruciate ligament (ACL)is one of the most commonly injured ligaments in the knee. Approximately 150,000 ACL injuries occur in the United States each year. Female athletes participating in basketball and soccer are two to eight times more likely to suffer an ACL injury compared to their male counterparts. Recent data from the Women’s National Basketball Association indicates white European-American players may be at increased risk for ACL injury compared with African-American, Hispanic or Asian players. Athletes who have suffered an ACL injury are at increased risk of developing arthritis later on in life, even if they have surgery for the injury. ACL injuries account for a large health care cost estimated to be over half-billion dollars each year.
WHY DO ACL INJURIES OCCUR?
Researchers believe there are external and internal factors associated with ACL injury. External factors include any play where the injured athlete’s coordination is disrupted just prior to landing or slowing down (deceleration). Examples of a disruption include being bumped by another player, landing in a pothole, or a ball deflection. Other external factors which have been studied include the effect(s) of wearing a brace, shoe-surface interface (how certain types of athletic footwear perform on different surfaces), and the playing surface itself. Internal factors include differences in the anatomy of men and women,increased hamstring flexibility, increased foot pronation (flat-footed), hormonal effects, and variations in the nerves and muscles which control the position of the knee. Anatomical differences between men and women, such as a wider pelvis and a tendency towards “knock knee” in women, may predispose women to ACL injury. Differences in ACL injury rates between men and women seem to begin shortly after puberty because the nerve/muscle system (coordination) adapts at a slower pace than the anatomical and hormonal changes. It is possible that the incidence of injuries in women increases at this age because the nerve/muscle system (coordination) adapts to these changes at a slower rate than in men. Women also tend to have knees that are less stiff than men, placing more forces on the ligaments. In addition, the female hormone estrogen may relax or allow stretching of the ACL, thereby predisposing female athletes to ACL injury. Nerve/muscle factors pertain to the interaction and control of the knee by the quadriceps and hamstrings muscles in the legs. Researchers are very interested in studying this particular factor since it may be the easiest to modify.
HOW DO ACL INJURIES OCCUR?
Careful study of videos of athletes tearing an ACL show that approximately 70 percent of these injuries are noncontact and 30 percent occur during contact. The noncontact injuries usually occur during landing or sharp deceleration. In these cases, the knee at the time of injury is almost straight and may be associated with valgus (inward) collapse (see Figure 1). The athlete often lands with a flat-foot position and the leg is placed in front or to the side of the trunk.
PREVENTION OF ACL INJURY
Several prevention programs have been developed in an attempt to decrease the incidence of noncontact ACL injuries. The focus of current prevention programs is on proper nerve/muscle control of the knee. These programs focus on plyometrics, balance, and strengthening/stability exercises. Plyometrics is a rapid, powerful movement which first lengthens a muscle (eccentric phase) then shortens it (concentric phase). The length-shortening cycle increases muscular power. An example would be an athlete jumping off a small box and immediately jumping back into the air after contact with the floor. Balance training commonly involves use of wobble or balance boards. On-field balance exercises may include throwing a ball with a partner while balancing on one leg. To improve single-leg core strength and stability, athletes perform exercises such as jumping and landing on one leg with the knee flexed and then momentarily holding that position.
PLYOMETRIC EXERCISES
High-intensity plyometrics may be key in reducing the number of ACL injuries. To be most successful, plyometric training should be performed more than once per week for a minimum of six weeks. Athletes are taught proper landing techniques which emphasize landing on the balls of the foot with the knees flexed and the chest over the knees (see Figure 2). The athlete should receive feedback on proper knee position to prevent inward buckling. Many of the newer programs are being adapted by coaches as an integral part of warm-up during practice, such as jumping over a soccer ball and landing in the correct position.
Information obtained from the American Orthopaedic Society for Sports Medicine, 2008.
The anterior cruciate ligament (ACL)is one of the most commonly injured ligaments in the knee. Approximately 150,000 ACL injuries occur in the United States each year. Female athletes participating in basketball and soccer are two to eight times more likely to suffer an ACL injury compared to their male counterparts. Recent data from the Women’s National Basketball Association indicates white European-American players may be at increased risk for ACL injury compared with African-American, Hispanic or Asian players. Athletes who have suffered an ACL injury are at increased risk of developing arthritis later on in life, even if they have surgery for the injury. ACL injuries account for a large health care cost estimated to be over half-billion dollars each year.
WHY DO ACL INJURIES OCCUR?
Researchers believe there are external and internal factors associated with ACL injury. External factors include any play where the injured athlete’s coordination is disrupted just prior to landing or slowing down (deceleration). Examples of a disruption include being bumped by another player, landing in a pothole, or a ball deflection. Other external factors which have been studied include the effect(s) of wearing a brace, shoe-surface interface (how certain types of athletic footwear perform on different surfaces), and the playing surface itself. Internal factors include differences in the anatomy of men and women,increased hamstring flexibility, increased foot pronation (flat-footed), hormonal effects, and variations in the nerves and muscles which control the position of the knee. Anatomical differences between men and women, such as a wider pelvis and a tendency towards “knock knee” in women, may predispose women to ACL injury. Differences in ACL injury rates between men and women seem to begin shortly after puberty because the nerve/muscle system (coordination) adapts at a slower pace than the anatomical and hormonal changes. It is possible that the incidence of injuries in women increases at this age because the nerve/muscle system (coordination) adapts to these changes at a slower rate than in men. Women also tend to have knees that are less stiff than men, placing more forces on the ligaments. In addition, the female hormone estrogen may relax or allow stretching of the ACL, thereby predisposing female athletes to ACL injury. Nerve/muscle factors pertain to the interaction and control of the knee by the quadriceps and hamstrings muscles in the legs. Researchers are very interested in studying this particular factor since it may be the easiest to modify.
HOW DO ACL INJURIES OCCUR?
Careful study of videos of athletes tearing an ACL show that approximately 70 percent of these injuries are noncontact and 30 percent occur during contact. The noncontact injuries usually occur during landing or sharp deceleration. In these cases, the knee at the time of injury is almost straight and may be associated with valgus (inward) collapse (see Figure 1). The athlete often lands with a flat-foot position and the leg is placed in front or to the side of the trunk.
PREVENTION OF ACL INJURY
Several prevention programs have been developed in an attempt to decrease the incidence of noncontact ACL injuries. The focus of current prevention programs is on proper nerve/muscle control of the knee. These programs focus on plyometrics, balance, and strengthening/stability exercises. Plyometrics is a rapid, powerful movement which first lengthens a muscle (eccentric phase) then shortens it (concentric phase). The length-shortening cycle increases muscular power. An example would be an athlete jumping off a small box and immediately jumping back into the air after contact with the floor. Balance training commonly involves use of wobble or balance boards. On-field balance exercises may include throwing a ball with a partner while balancing on one leg. To improve single-leg core strength and stability, athletes perform exercises such as jumping and landing on one leg with the knee flexed and then momentarily holding that position.
PLYOMETRIC EXERCISES
High-intensity plyometrics may be key in reducing the number of ACL injuries. To be most successful, plyometric training should be performed more than once per week for a minimum of six weeks. Athletes are taught proper landing techniques which emphasize landing on the balls of the foot with the knees flexed and the chest over the knees (see Figure 2). The athlete should receive feedback on proper knee position to prevent inward buckling. Many of the newer programs are being adapted by coaches as an integral part of warm-up during practice, such as jumping over a soccer ball and landing in the correct position.
Information obtained from the American Orthopaedic Society for Sports Medicine, 2008.
Thursday, June 20, 2013
Orthopedic Surgery at St. Louis Children's Hospital is ranked 6th in the nation by US News and World Report
Orthopedic Surgery at St. Louis Children's Hospital is ranked 6th in the nation by US News and World Report. Learn more here: http://health.usnews.com/best-hospitals/area/mo/st-louis-childrens-hospital-6631180
Tuesday, June 11, 2013
Senior Focus: Protecting knees to prevent or slow osteoarthritis
Researchers estimate that more than 10 percent of the population (27 million Americans) have some osteoarthritis.
This condition is associated with more than 7 million annual visits to doctors. Initial symptoms are pain with activities. However, as arthritis progresses, continuous pain even while at rest can occur.
Potential risk factors for knee osteoarthritis include obesity, older age and prior knee injury or surgery. Knee osteoarthritis cannot be cured completely, but many strategies can be used to slow its progression.
Obese patients have a higher rate of knee osteoarthritis, and moderate weight loss may reduce the incidence of knee osteoarthritis by 50 percent. Thus, lifestyle modifications that include a healthy diet and weight loss may protect the knee joint from disease progression.
Read more here
This condition is associated with more than 7 million annual visits to doctors. Initial symptoms are pain with activities. However, as arthritis progresses, continuous pain even while at rest can occur.
Potential risk factors for knee osteoarthritis include obesity, older age and prior knee injury or surgery. Knee osteoarthritis cannot be cured completely, but many strategies can be used to slow its progression.
Obese patients have a higher rate of knee osteoarthritis, and moderate weight loss may reduce the incidence of knee osteoarthritis by 50 percent. Thus, lifestyle modifications that include a healthy diet and weight loss may protect the knee joint from disease progression.
Read more here
Tuesday, April 23, 2013
Plantar Fasciitis
WHAT IS PLANTAR FASCIITIS?
Plantar fasciitis is pain felt at the bottom of the heel. It is usually felt on the first step out of bed in the morning or when walking again after resting from a walking or running activity. However, plantar fasciitis pain can, if it persists, soon be felt any time you are walking, running or jumping. Although the pain is mostly felt at the bottom of the heel, it can also radiate down the entire bottom of the foot toward the toes. Plantar fasciitis is not usually associated with numbness or tingling.
ANATOMY OF THE PLANTAR FASCIA
The plantar fascia consists of dense bands of tissue deep below the skin that extend out in a fan-like fashion from the heel bone to the toes. If you pull your toes and foot toward your head, you will feel this tissue tighten.
WHAT CAUSES PLANTAR FASCIITIS?
Plantar fasciitis is thought to be caused by repetitive stretching of the tight bands of the plantar fascia which result in micro tears in these bands as they extend from the heel. Because these tears usually do not occur from a single traumatic event, an immediate healing reaction is not triggered. A chronic irritation or inflammation process thereby begins which increases with activity. A sudden weight gain may also increase stress to an otherwise normal plantar fascia. Pulling of the tight plantar fascia on the heel bone during activity can result in the formation of a bone spur off the tip of the heel bone, at the origin of the plantar fascia tissue. This bone spur itself is not the cause of pain, but rather the mechanical result of the chronic inflammatory process on the bone caused by the stretching of the tight tissue.
TREATMENT TIPS
Surgery is rarely necessary to treat plantar fasciitis. To decrease your pain and symptoms, you may want to:
Information obtained from the American Orthopaedic Society for Sports Medicine, 2008.
Plantar fasciitis is pain felt at the bottom of the heel. It is usually felt on the first step out of bed in the morning or when walking again after resting from a walking or running activity. However, plantar fasciitis pain can, if it persists, soon be felt any time you are walking, running or jumping. Although the pain is mostly felt at the bottom of the heel, it can also radiate down the entire bottom of the foot toward the toes. Plantar fasciitis is not usually associated with numbness or tingling.
ANATOMY OF THE PLANTAR FASCIA
The plantar fascia consists of dense bands of tissue deep below the skin that extend out in a fan-like fashion from the heel bone to the toes. If you pull your toes and foot toward your head, you will feel this tissue tighten.
WHAT CAUSES PLANTAR FASCIITIS?
Plantar fasciitis is thought to be caused by repetitive stretching of the tight bands of the plantar fascia which result in micro tears in these bands as they extend from the heel. Because these tears usually do not occur from a single traumatic event, an immediate healing reaction is not triggered. A chronic irritation or inflammation process thereby begins which increases with activity. A sudden weight gain may also increase stress to an otherwise normal plantar fascia. Pulling of the tight plantar fascia on the heel bone during activity can result in the formation of a bone spur off the tip of the heel bone, at the origin of the plantar fascia tissue. This bone spur itself is not the cause of pain, but rather the mechanical result of the chronic inflammatory process on the bone caused by the stretching of the tight tissue.
TREATMENT TIPS
Surgery is rarely necessary to treat plantar fasciitis. To decrease your pain and symptoms, you may want to:
- Tape the heel and arch. Custom shoe inserts may be needed to support the arch and the heel. Increase the flexibility of the plantar fascia and calf muscles by doing stretching exercises. Tight calf muscles increase he stress on the plantar fascia and predispose you to plantar fasciitis.
- Massage the plantar fascia by rolling your foot over a round tubelike object with a diameter of 3 to 4 inches. A rolling pin works nicely for this. Strengthen the muscles of the foot and ankle that support the arch. One way to do this is to scrunch up a hand towel with your toes or use your toes to pull a towel weighted with a food can across the floor.
- Warm up well before stretching. Cold tissues cannot stretch as effectively. After stretching, ice your heel for 20 to 30 minutes at the point of maximum tenderness to decrease any inflammation that may result from too vigorous a workout.
- Consider the use of oral antiinflammatory medications such as aspirin or ibuprofen. These medications can decrease the inflammation of the plantar fascia and thus decrease your symptoms so that you can stretch and improve your flexibility. In some cases, your physician may recommend a prescription antiinflammatory for you.
- Try a night splint. These devices, prescribed by your physician, keep the foot flexed at 90 degrees instead of the typical relaxed foot position of toes pointed down that occurs during sleep. Wearing a splint may lessen the pain of the first step in the morning.
- Massage the heel with a sports cream, which may lessen symptoms. A variety of “hands on” therapeutic treatments can also be administered by a physical therapist.
- Always warm up well and stretch before participating in sports.
- Wear good, supportive shoes for your athletic activities.
- Keep the muscles of your feet and ankles strong to support your arch.
- Don’t try running to lose weight after a rapid weight gain. Walk first, and stretch the muscles of the foot and calf to help condition your body before running.
- Avoid activities that cause pain in your heel.
Information obtained from the American Orthopaedic Society for Sports Medicine, 2008.
Thursday, April 18, 2013
Thursday, April 4, 2013
Dr. Klein on Choosing the Correct Shoes for Spring and Summer
Spring is here with warmer weather, outdoor activities and our favorite sandals. Frequently, foot pain and problems are a direct result of the shoes we choose. These tips can help keep your feet safe in the spring and summer months.
• Warm weather often encourages us to participate in new activities. While outdoor activities are a healthy pursuit, be careful when starting something new. You should make sure the shoes you wear are appropriate for the particular sport or activity. Overuse injuries are frequently seen in the foot and ankle when you try to do too much of one activity after a long winter. Start slowly and increase your activity as you become stronger, and your endurance increases.
• Flip-flops rule at the pool. Many patients ask weather flip-flops are safe to wear, and the answer is no. When protecting your feet from hot pavement at poolside, flip-flops are an excellent choice. Flip-flops can actually help strengthen feet, and are best worn on flat, reliable surfaces. When you head to the local amusement park for a day of walking or the closest skate park for an outdoor hike, opt for sturdier, more supportive footwear. Long periods of walking and extensive walking on uneven ground with flip-flops or any open-back sandal can cause injury to the foot.
• Stylish sandals and shoes for men can offer minimal support, and risk injury to the foot and ankle when worn for inappropriate activities. While there is no harm to wearing these shoes to a casual barbecue or dinner party, you may cause injury to your foot if you decide to hop on a bike or participate in the unexpected softball game. Wearing your favorite summer dress shoes should be limited to activities that require a low level of activity.
Choose the shoe to match the activity. Keep a pair of supportive athletic shoes and socks in the car, so you are ready for anything – and enjoy the weather.
Monday, March 25, 2013
Leesa Galatz, MD: Muscle Transfer Operation as New Treatment for Rotator Cuff Injuries
 |
| Leesa M. Galatz, MD, associate professor of orthopaedic surgery, performing a post-operative exam on surgery patient Margaret Engelman. |
Leesa Galatz, MD, a shoulder and elbow specialist at Washington University Orthopedics, was recently featured in an article for the Record, a Washington University publication. Dr. Galatz discusses muscle transfer operation, a groundbreaking surgical technique used in the treatment of chronic rotator cuff disease.
Read the full story here: https://news.wustl.edu/news/Pages/25146.aspx
Original article written by Jim Dryden
Monday, March 18, 2013
Center for Adolescent & Young Adult Hip Disorders
 |
| Center for Adolescent and Young Adult Hip Disorders Team (from left): Ryan Nunley, MD; Heidi Prather, DO; Mark Halstead, MD; John Clohisy, MD; Perry Schoenecker, MD; Devyani Hunt, MD; Robert Barrack, MD; J. Eric Gordon, MD. NOT PICTURED: James Keeney, MD |
Young adult hip disorders are one of the most rapidly advancing subspecialties in orthopedics. Washington University Orthopedics offers the Center for Adolescent and Young Adult Hip Disorders, which focuses exclusively on providing comprehensive and specialized care to adolescents and young adults with hip disorders, and is committed to seeing each patient expeditiously.
Center director John Clohisy, MD, and Perry Schoenecker, MD, work in conjunction with the pediatric orthopedic service, physiatrists, adult reconstructive surgeons, physical therapists and a dedicated staff of nurses and medical assistants to form an extremely experienced team with the expertise to accurately diagnose and deliver the full spectrum of both non-surgical and surgical solutions. Commonly, these young patients are athletes and we are fully committed to returning them to their sport and recreational activities.
Read more about our Center for Adolescent and Young Adult Hip Disorders.
Thursday, March 7, 2013
Tuesday, March 5, 2013
Tanya Strautmann - Hip Labral Tear
In her 12 years with the St. Louis Ballet company — during which time
she danced many lead roles and rose to international acclaim —
principal ballerina Tanya Strautmann had missed only one day of class
and performing. So when hip pain forced her to take two days off in the
Spring of 2008, she knew she had crossed the threshold from what she
calls “good pain” into “bad pain.”
 “Dancers always have aches, but as I tried to push through, I
eventually knew that something was not right.” After the two days off,
she returned to class and “couldn’t do anything,” she says.
“Dancers always have aches, but as I tried to push through, I
eventually knew that something was not right.” After the two days off,
she returned to class and “couldn’t do anything,” she says.Visits to several doctors were unproductive, primarily, she believes, because many physicians can’t fully appreciate the movement required of dancers. “A long-distance runner’s knee might be the most challenging case most doctors see,” but a much wider range of graceful movement is required of a ballerina, and treating a dancer “takes a special awareness,” she says.
Then Strautmann recalled a lecture she had heard by Devyani Hunt, MD, and her colleagues in the Medical Program for Performing Artists group at Washington University School of Medicine’s Department of Orthopaedic Surgery. Hunt, assistant professor of orthopaedic surgery and a specialist in physical and rehabilitative medicine, also is a dancer. “She understands a dancer’s needs and speaks the language,” Strautmann says, “so when I say ‘developpe,’(a movement in which the working leg is drawn up to the knee of the supporting leg, then smoothly out into the air) she knows precisely the motion I’m describing.”
After X-rays ruled out arthritis and revealed that no bone had been fractured, Hunt suspected that Strautmann may have suffered a hip labral tear, an injury in which the ring of protective cartilage around the outside rim of the hip socket is damaged. Pain and limited range of motion are common symptoms of a labral tear, and athletes and dancers who engage in repetitive twisting or pivoting motions often are affected. Continue reading Tanya's story here
Thursday, February 28, 2013
Cervical Disc Herniation
Learn more about cervical disc herniation from spine surgeon Dr. Jacob Buchowski.
Monday, February 18, 2013
Scoliosis Frequently Asked Questions
Why does scoliosis develop most often in late childhood?
Why is it more common in girls? Scoliosis most often develops in late childhood because of the association between growth and progressive scoliosis curves. Although scoliosis can develop at any age, including infantile (age birth- 3), Juvenile (age 3-10), adolescent (age 10-18) and adult (> age 18), the most common time to detect curves are in late childhood/early teen years. Thus, the most common form seen, Adolescent Idiopathic Scoliosis (AIS), is detected between ages 10 and 18, often just before or after puberty and the associated adolescent growth spurt. Small curves (10-20 degrees) are nearly equally found in boys and girls, but larger curves which often need treatment (those > 40 degrees) are seen in females to males in a 9:1 ratio. It is a bit unclear why that is the case, it may certainly be a genetic tendency, and/or something relating to hormonal alterations or connective tissue adaptations for the potential for childbirth in females.
What causes some children to develop scoliosis while others do not?
Is it simply genetic or are there other factors involved? Although there are many potential etiologic factors implicated for idiopathic scoliosis development, the genetic aspects are probably the most influential. Multiple genetic studies have confirmed strong family relations including studies of identical vs paternal twins. Other factors such as various hormones, equilibrium and balance issues have been promoted as well, but none are conclusive. The genetic factors are strong but highly complex, multigene interactions that are still being actively investigated, including here at Washington University by Dr Matt Dobbs of the Department of Orthopedic Surgery.
What causes adults to develop scoliosis?
Adults can develop scoliosis as a result of slow progression of childhood curves that were untreated, or as curves that develop on their own from aging of the spine, usually in the lower (lumbar) region and termed "de novo" adult lumbar scoliosis. These de novo curves result from progressive degeneration of the joints in the back of the spine along with degeneration of the discs supporting the front of the spine. Although this natural aging process occurs in everyone, only certain people will develop a corresponding scoliosis with the process.
To read more Scoliosis FAQ's, please visit our website at: http://www.ortho.wustl.edu/content/Patient-Care/3319/SERVICES/Spine/Scoliosis-FAQ.aspx.
Why is it more common in girls? Scoliosis most often develops in late childhood because of the association between growth and progressive scoliosis curves. Although scoliosis can develop at any age, including infantile (age birth- 3), Juvenile (age 3-10), adolescent (age 10-18) and adult (> age 18), the most common time to detect curves are in late childhood/early teen years. Thus, the most common form seen, Adolescent Idiopathic Scoliosis (AIS), is detected between ages 10 and 18, often just before or after puberty and the associated adolescent growth spurt. Small curves (10-20 degrees) are nearly equally found in boys and girls, but larger curves which often need treatment (those > 40 degrees) are seen in females to males in a 9:1 ratio. It is a bit unclear why that is the case, it may certainly be a genetic tendency, and/or something relating to hormonal alterations or connective tissue adaptations for the potential for childbirth in females.
What causes some children to develop scoliosis while others do not?
Is it simply genetic or are there other factors involved? Although there are many potential etiologic factors implicated for idiopathic scoliosis development, the genetic aspects are probably the most influential. Multiple genetic studies have confirmed strong family relations including studies of identical vs paternal twins. Other factors such as various hormones, equilibrium and balance issues have been promoted as well, but none are conclusive. The genetic factors are strong but highly complex, multigene interactions that are still being actively investigated, including here at Washington University by Dr Matt Dobbs of the Department of Orthopedic Surgery.
What causes adults to develop scoliosis?
Adults can develop scoliosis as a result of slow progression of childhood curves that were untreated, or as curves that develop on their own from aging of the spine, usually in the lower (lumbar) region and termed "de novo" adult lumbar scoliosis. These de novo curves result from progressive degeneration of the joints in the back of the spine along with degeneration of the discs supporting the front of the spine. Although this natural aging process occurs in everyone, only certain people will develop a corresponding scoliosis with the process.
To read more Scoliosis FAQ's, please visit our website at: http://www.ortho.wustl.edu/content/Patient-Care/3319/SERVICES/Spine/Scoliosis-FAQ.aspx.
Tuesday, February 12, 2013
Thursday, February 7, 2013
Outpatient Spine Center
This month, we are featuring spine health. Spine specialists with Washington University Orthopedics
are nationally and internationally renowned for treating adult and pediatric patients with a wide range of
spinal diseases and conditions of the cervical, thoracic, and lumbar
spine.
At the Washington University Orthopedic Outpatient Spine Center in Chesterfield, Missouri, spine surgery is a last resort. Click here to learn more about our Orthopedic Spine Center Clinicians:
http://www.ortho.wustl.edu/content/Patient-Care/3037/SERVICES/Spine/Orthopedic-Spine-Center-for-Back-Pain/Meet-Our-Clinicians.aspx
At the Washington University Orthopedic Outpatient Spine Center in Chesterfield, Missouri, spine surgery is a last resort. Click here to learn more about our Orthopedic Spine Center Clinicians:
http://www.ortho.wustl.edu/content/Patient-Care/3037/SERVICES/Spine/Orthopedic-Spine-Center-for-Back-Pain/Meet-Our-Clinicians.aspx
Tuesday, January 29, 2013
Learn about work-related injuries of the hand
Thursday, January 24, 2013
Thursday, January 17, 2013
Monday, January 14, 2013
Caring for your Hands, Wrists and Elbows
Tuesday, February 5th, 6:30 pm to 8:30 pm
Do you have a hand or wrist condition that you would like to speak to one of our physicians about? Join us at our community event on February 5th, and spend the evening learning how to keep your hands healthy with doctors you can trust. Washington University Orthopedics Peterson Hand Center specialists will present on common hand, wrist and elbow topics.
• Speak one-on-one with Washington University physicians
• Perfect your golf swing and test your hand-grip strength
• Relax with complimentary hand massages, paraffin wax
treatments and mini-manicures
• Enjoy light refreshments
The event is free, but registration is required. To register, please call 314-TOP-DOCS (314-867-3627) or toll-free 866-867-3627. For more information regarding the event, please visit: http://
Tuesday, February 5th, 6:30 pm to 8:30 pm
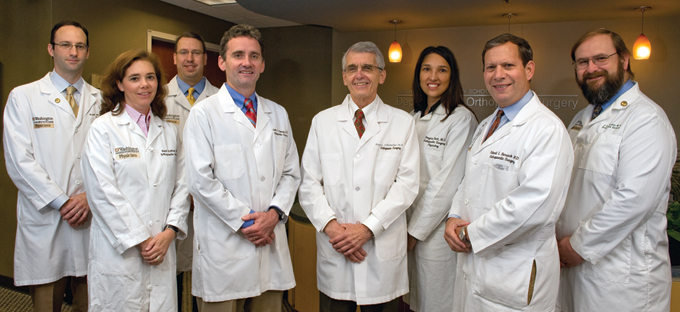
Peterson Hand Center Physicians featured above (from left):
Martin Boyer, MD, FRCS(C), Daniel Osei, MD, Ryan Calfee, MD, MSc, Lindley Wall, MD, Richard Gelberman, MD, Charles Goldfarb, MD
Martin Boyer, MD, FRCS(C), Daniel Osei, MD, Ryan Calfee, MD, MSc, Lindley Wall, MD, Richard Gelberman, MD, Charles Goldfarb, MD
Do you have a hand or wrist condition that you would like to speak to one of our physicians about? Join us at our community event on February 5th, and spend the evening learning how to keep your hands healthy with doctors you can trust. Washington University Orthopedics Peterson Hand Center specialists will present on common hand, wrist and elbow topics.
• Speak one-on-one with Washington University physicians
• Perfect your golf swing and test your hand-grip strength
• Relax with complimentary hand massages, paraffin wax
treatments and mini-manicures
• Enjoy light refreshments
The event is free, but registration is required. To register, please call 314-TOP-DOCS (314-867-3627) or toll-free 866-867-3627. For more information regarding the event, please visit: http://
Subscribe to:
Comments (Atom)



